Sleep apnea is a sleeping disorder that creates a breathing fluctuation while sleeping. CPAP masks are machines that help CPAP users to sleep comfortably. Several kinds of sleep apnea masks have assisted people in having a night of quality sleep. CPAP mask categories have different components that can rectify the OSA.
The best CPAP mask has been an outstanding solution to any OSA out of other solutions. However, some people who snore heavily are not enjoying sleep such needs therapy and treatment. Some of the symptoms of sleep apnea are sleeping during the daytime and snoring. You can’t have quality time sleeping when you experience a disruption in breathing. This sleep apnea experience can cause colossal health damage when it is not given attention and quality treatment.

You must visit any sleep therapist or specialist to diagnose the kind of OSA you have and know the treatment approach to adopt. In this article, you will be opened to the causes of OSA, the mask types, and the best CPAP mask that will give you the comfort you desire and also need to see CPAP therapy.
Causes of Obstructive Sleep Apnea
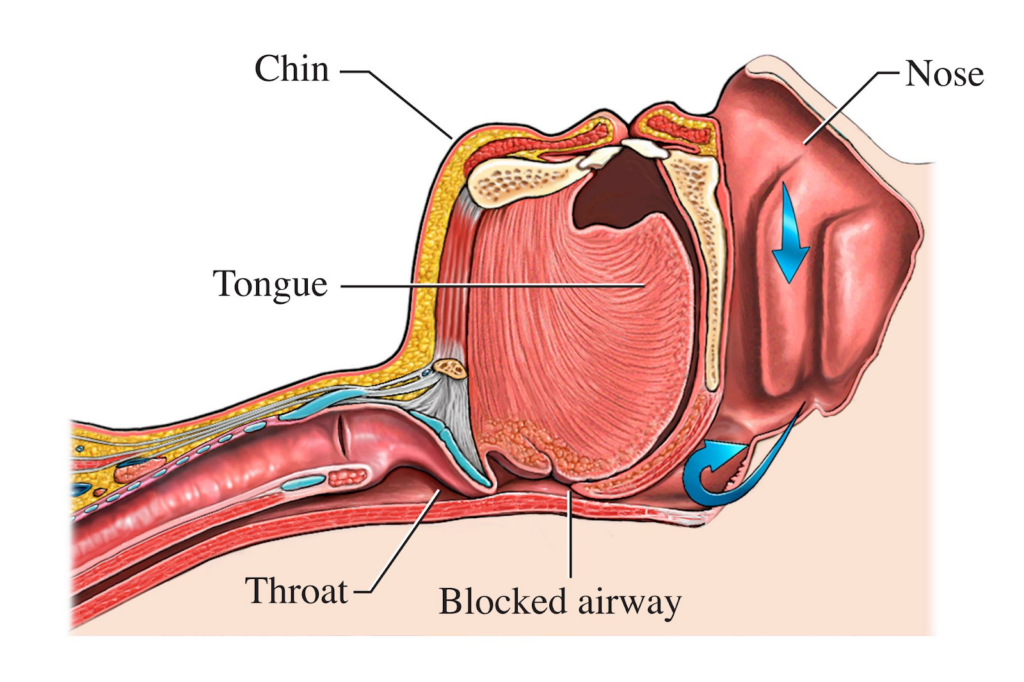
So many factors are responsible for a sleep disorder; in this section, we’ll consider some factors and how to tackle them with a CPAP mask.
Gender
Most of the time, men are more likely to have OSA. Gender also affects who can easily have sleep issues due to some sex hormones. Though women also have OS only after menopause
Diabetes
People with diabetes can easily have OSA. Diabetes can also affect the rate of how breathing which can cause sleeplessness
Smoking

Smoking is so detrimental to health that it can also cause OSA. Smoking can also affect the throat; when the throat is concerned, the airway may not be open, which can affect
Nasal congestion
Nasal congestion creates a narrow airway due to consistent congestion in the nostrils. It will affect breathing capacity and can even result in headaches, body pain, and sleeplessness.
Obesity
Though not all who are overweight have a sleep disorder, most of them experience sleeping disorders because too much fat in the body can block air passage. Also, there are conditions such as Obesity which is polycystic, and hypothyroidism can cause sleep disorders.
Age
Some ages are very close to having OSA because of some hormones in the body, but at the 60s upward, the chances of having sleep disorder decrease.
Glaucoma

This eye problem also can cause sleep disorders due to the connection of the eyes to the head. There are many complications, but CPAP masks can solve this problem.
Hormone disorder

Some hormone conditions can also cause or increase the chances of having OSA. Some of the growth tissue can as well block the airway, which can later develop into a sleep disorder
Sleeping position
Some sleeping positions are very risky to the health, especially the back sleeper; such sleeping style may affect the airway and eventually affect d breathing. These factors and many more are potential agents that can cause OSA. Meanwhile, all the elements can be treated and avoided with the help of CPAP therapy and a sleep specialist. Finally, I will briefly discuss CPAP masks and other accessories and how they can be administered to anyone with a sleep disorder.
CPAP Masks and their Uses.
This CPAP mask is a carrier for air pressure to the airway to assist the person with sleep Apnea to breathe comfortably while sleeping on the bed. There are different sizes and styles of CPAP masks, and the materials used in making the masks are also different. Out of the CPAP masks outside, only three are shared, widely accepted, and recommended by the sleep therapist.
They are
- Nasal pillow masks
- Full face masks
- Nasal masks
These CPAP masks are differently molded and work differently but have the same result.CPAP machines are the most recommended and effective treatment for sleep disorders. In addition, some other important CPAP mask components are essential to treating obstructed sleep.
- Nasal pillows
- Nasal cradle cushion
- Silicone cushion
- Chin strap
- Adaptive frame
- Mask fits
- Glasses
- Face mask
- Headgear
All these are very important, and they give comfort to anyone who is battling with OSA. However, using a CPAP mask depends on how your therapist explains it. Applying the CPAP mask is straightforward but must be according to the explanation of your therapy.
There are steps to follow when using the CPAP mask. First, whichever of the masks you prescribe, you must ask your therapist how to install and use it. Next, let’s discuss some of the methods for using CPAP masks.
First and foremost, you must find an excellent place to keep your CPAP machines. When your machine is safe, every other component, like the hose and the mask, will function well. The device must be closer to your bed for easy plugging at night.
The filter is also necessary to always check and follow the instruction given to you by your sleep therapist. The filter can be changed anytime, but there is a method of removing and fixing it. Connecting the hose to the CPAP is easy as long as you can read the manual that comes with the CPAP machine, and more so, you can adhere to how your doctor informed you.
In addition, the connectivity between the hose to the mask is also easy. The hose is connected to the CPAP mask, leaving no space for air to escape. Your sleep doctor determines the mask you will be putting on—based on your breathing, your sleeping position, and your type of OSA.
Some face masks cover the entire face, some only cover the nose, while others cover the nose and mouth. Wearing the mask is accessible as much as you have the right face mask. You will also need straps to help tighten the mask around your head, which must comfortably fit in. The fixing of the strap must not be painful to breathe comfortably.
Conclusion
Many things are potential agents that cause obstructive sleeping. But the OS can be corrected with sleep therapy, CPAP masks, and other components. When this sickness is not treated right, it damages health. So with the knowledge of what causes sleep apnea, one must see their doctor to know what to do. Do not only focus on the problem alone but look for the solution and enjoy your sleep.
Also read:
- How an Oxygen Compressor Can Improve Your Home Oxygen Therapy Experience
- How CPAP Machines Improve Sleep Quality and Prevent Sleep Apnea Complications
- Buy CPAP Mask Australia: Affordable Options for Every Budget
- CPAP Masks Australia: A Complete Guide for Buyers
- Alternative Sleep Apnea Treatments for Those Who Can’t Tolerate CPAP